Clinical Evidence
Proprietary Mepilex® Border is the only 5-layer foam dressing for which over 80 evidence pieces exist to support its effectiveness in preventing pressure ulcers.
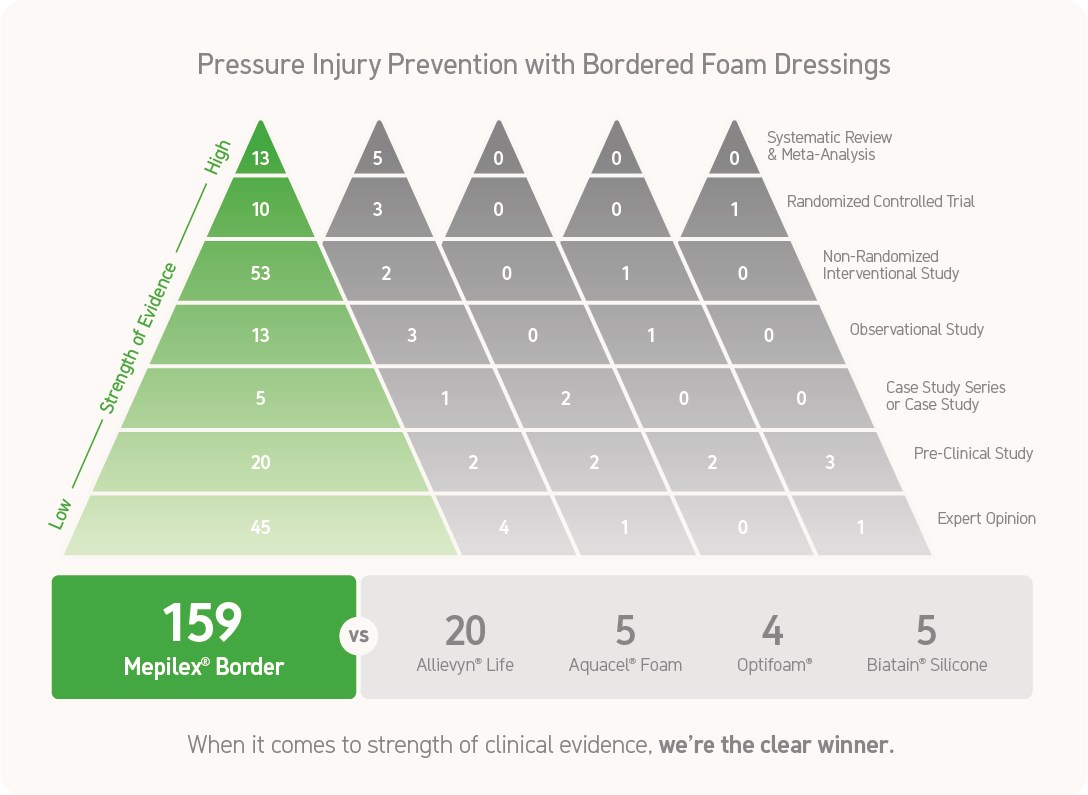
In fact, Mepilex Border is the only 5-layer foam dressing with 4 peer reviewed and published RCTs showing its isolated effectiveness in pressure ulcer prevention.
View our key evidence:
Clinical Practice Guidelines / Health Technology Assessment
Dressings as an adjunct to pressure ulcer prevention: consensus panel recommendations. International Wound Journal 2014;doi:10/1111/iwj.12197.
Abstract:
The formulation of recommendations on the use of wound dressings in pressure ulcer prevention was undertaken by a group of experts in pressure ulcer prevention and treatment from Australia, Portugal, UK and USA. After review of literature, they concluded that there is adequate evidence to recommend the use of five-layer silicone bordered dressings (Mepilex® Border Sacrum) and 3 layer Mepilex®Heel dressings by Mölnlycke Health Care, Gothenburg, Sweden) for pressure ulcer prevention in the sacrum, buttocks and heels in high-risk patients, those in emergency department (ED), intensive care unit (ICU) and operating room (OR). Literature on which this recommendation is based includes one prospective randomized control trial, three cohort studies and two case series. Recommendations for dressing use in patients at high risk for pressure injury and shear injury were also provided.
https://www.ncbi.nlm.nih.gov/pubmed/24588955
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers: Clinical Practice Guideline. Haesler, E. (eds). Cambirdge Media, Perth, Australia, 2014.
This guideline is the result of a collaborative effort among the National Pressure Ulcer Advisory Panel (NPUAP), European Pressure Ulcer Advisory Panel (EPUAP) and Pan Pacific Pressure Injury Alliance (PPPIA). A comprehensive literature review was conducted on pressure ulcer prevention and treatment. A rigorous scientific methodology was used to appraise available research and make evidence-based recommendations for the prevention and treatment of pressure ulcers.
The guideline includes 575 explicit recommendations and/or research summaries for the following pressure ulcer topics: etiology; prevalence and incidence; risk assessment; skin and tissue assessment; preventive skin care; prophylactic dressings; microclimate control; fabrics and textiles; nutrition; repositioning and early mobilization; support surfaces; medical device related pressure ulcers; pressure ulcer classification; wound assessment; monitoring of healing; pain assessment and treatment; cleansing; debridement; wound dressings (including growth factors and biological wound dressings); assessment and treatment of infection and biofilms; biophysical agents (e.g. electrical stimulation, negative pressure wound therapy, electromagnetic field treatment); and surgery.
http://www.npuap.org/resources/educational-and-clinical-resources/prevention-and-treatment-of-pressure-ulcers-clinical-practice-guideline/
World Union of Wound Healing Societies (WUWHS) Consensus Document. Role of dressings in pressure ulcer prevention. Wounds International, 2016.
Overview:
Recognition of the huge economic, health-related and social burden of pressure ulcers has resulted in considerable efforts to reduce their occurrence. Despite this, pressure ulcers still occur. In recent years, evidence has been building that some types of dressings typically used to treat open wounds have the potential to supplement standard pressure ulcer prevention measures and further reduce incidence.
http://www.woundsinternational.com/wuwhs/view/consensus-document-role-of-dressings-in-pressure-ulcer-prevention
Systematic Reviews
Clark M, Black J, Alves P, Brindle C, Call E, Dealey C, Santamaria N. Systematic review of the use of prophylactic dressings in the prevention of pressure ulcers. International Wound Journal 2014;11(5):460-471.
Tayyib N, Coyer F. Effectiveness of pressure ulcer prevention strategies for adult patients in intensive care units: a systematic review. Worldviews on Evidence-Based Nursing 2016;13(6):432-444.
Monograph
Davies P. Role of multi-layer foam dressings with Safetac in the prevention of pressure ulcers: a review of the clinical and scientific data. J Wound Care 2016; 25: 1, S1–S24.
Randomized Clinical Trials
Aloweni F, Lim, ML, Chua TL, Tan SB, Lian, SB, Ang SY. A randomised controlled trial to evaluate the incremental effectiveness of a prophylactic dressing and fatty acids oil in the prevention of pressure injuries. Wound Practice and Research 2017;25(1):24-34.
Kalowes P, Messina V, Li, M. Five-layered soft silicone foam dressing to prevent pressure ulcers in the intensive care unit. American Journal of Critical Care 2016;25(6):e108-e119.
Santamaria N, Gerdtz M, Sage S, McCann J, Freeman A, Vassiliou T, De Vincentis S, Ng AW, Manias E, Liu W, Knott, J. A randomised controlled trial of the effectiveness of soft silicone multi-layered foam dressings in the prevention of sacral and heel pressure ulcers in trauma and critically ill patients: the border trial. International Wound Journal 2013; doi: 10.1111/iwj.12101.
Tsao W-Y, Lo S-F, Harmod T, Lee R-P. A comparison of the efficacy of different wound dressing management techniques in preventing pressure ulcers. Journal of Nursing (China) 2013;60(4):65-78.
Non-Randomized Clinical Trials
Baker G. Nursing driving excellence: preventing pressure ulcers in the high-risk population. Poster presentation at the Symposium on Advanced Wound Care Fall, Las Vegas, Nevada, United States of America, 2014.
Bender J, Kenyon D, Johnson C, Mariani S. Pressure injury prevention begins in the emergency room. Poster presentation at National Pressure Ulcer Advisory Panel Biennial Conference, New Orleans, Louisiana, United States of America, 2017.
Black JM, Kalowes P. Medical device-related pressure ulcers. Chronic Wound Care Management and Research 2016;3:91-99.
Brindle CT. Outliers to the Braden Scale: identifying high-risk ICU patients and the results of prophylactic dressing use. World Council of Enterostomal Therapists Journal 2010; 30 (1): 11-18.
Brindle CT, Wegelin, J.A. Prophylactic dressing application to reduce pressure ulcer formation in cardiac surgery patients. Journal of Wound Ostomy & Continence Nursing 2012; 39(2):133-142.
Byars M, Raxter K, Reed-Chism, R. How to prevent pressure ulcers on a kinetic therapy support surface. Poster presentation at the Joint Conference of the Wound Ostomy and Continence Nurses Society and the World Council of Enterostomal Therapists, New Orleans, Louisiana, United States of America, 2011.
Byrne J, Nichols P, Sroczynski M, Stelmaski L, Stetzer M, Line C, Carlin K. Prophylactic sacral dressing for pressure ulcer prevention on high-risk patients. American Journal of Critical Care 2016;25(1):228-234.
Cano A, Smits D, Corvino P. Efficacy of the prohylactic use of silicone foam dressing for the prevention of pressure ulcers in patients: an observational study in a 24 bed cardiovascular and cardiac intensive care unit. Journal of Wound, Ostomy and Continence Nursing 2011;38(3S):S73.
Castelino I, Mercer D, Forrest Calland J. Reducing peri-operative pressure ulcers in thoracic, cardiovascular, and spinal surgery patients: achieving zero incidence is possible! Poster presentation at the Symposium on Advanced Wound Care (Spring), Atlanta, Georgia, 2012.
Chaiken N. Reduction of sacral pressure ulcers in the intensive care unit using a silicone border foam dressing. Journal of Wound Ostomy & Continence Nursing 2012;39(2):143-145.
Cherry C, Midyette P. The Pressure Ulcer Prevention Care Bundle: a collaborative approach to preventing hospital-acquired pressure ulcers. Poster presentation at Magnet Research Day, Alabama, United States of America, 2010.
Coakley K, Downs B. Take it to zero: a process improvement project for reducing pressure ulcer rates. Poster presentation at the 12th Biennial National pressure Ulcer Advisory Panel Congress, Norfolk, Virginia, United States of America, 2011.
Cooper M, Godke J, Nasca J. Bundling for change: implementing pressure injury prevention. Poster presentation at 49th Annual Conference of the Wound, Ostomy and Continence Nurses Society, Salt Lake City, Utah, United States of America, 2017
Gentry T, Wright A. The 'Sacral Heart' dressing study: use of an absorbent self-adherent soft silicone sacral foam dressing across acute care settings. Poster presentation at the Joint Conference of the Wound Ostomy and Continence Nurses Society and the World Council of Enterostomal Therapists, Phoenix, Arizona, United States of America, 2010.
Haisley V, Potter K, Wallace J, George R, Betsill K. An ounce of prevention: the use of an absorbent soft silicone self-adherent bordered foam heel dressing to decrease the incidence of hospital-acquired heel pressure ulcers in an acute care setting. Poster presentation at Wound Ostomy and Continence Nurses' Society conference, San Antonio, Texas, United States of America, 2015.
Johnstone A, McGown K. Innovations in the reduction of pressure ulceration and pain in critical care. Wounds UK 2013;9(3):76-80.
Kalowes P, Messina V, Paige R. Reducing medical device related pressure ulcers. An interprofessional approach using data & innovation to improve adult & pediatric outcomes. Poster presentation at the Symposium on Advanced Wound Care Fall, Las Vegas, Nevada, United States of America, 2014.
Kiely C. Cultural transformation in pressure ulcer prevention and care. Journal of Wound Ostomy and Continence Nursing 2012; 39 (4): 443-446.
Kimsey D, Flannigan C, Quill J. A formal process for reducing the risk of perioperative pressure injury. Poster presentation at Association of periOperative Registered Nurses Global Surgical Conference & Expo, Boston, Massachusetts, United States of America, 2017.
Koerner S, Adams D. Save our sacrums (S.O.S.) Does the use of an absorbent soft silicone self-adherent bordered foam dressing decrease the incidence of hospital acquired pressure ulcers? Poster presentation at the Joint Conference of the Wound Ostomy and Continence Nurses Society and the World Council of Enterostomal Therapists, New Orleans, Louisiana, United States of America, 2011.
Muldoon C, Grossman N, Lawrence P. Initial use absorbent soft silicone self-adherent bordered foam dressing reduces sacral pressure ulcers in the cardiovascular ICU. Poster presentation at the Joint Conference of the Wound Ostomy and Continence Nurses Society and the World Council of Enterostomal Therapists, Phoenix, Arizona, United States of America, 2010.
Ordona RB, Kirkland-Walsh H. Fixed it! Protecting against device related pressure ulcers. Poster presentation at Wound Ostomy and Continence Nurses Society and Canadian Association for Enterostomal Therapy, Montreal, Canada, 2016.
Padula WV. Effectiveness and value of prophylactic 5-layer foam sacral dressings to prevent hospital-acquired pressure injuries in acute care hospitals. An observational cohort study. Journal of Wound Ostomy and Continence Nursing 2017;44(5):1-6 [Epub ahead of print].
Park KH. The effect of a silicone border foam dressing for prevention of pressure ulcers and incontinence associated dermatitis in intensive care unit patients. Journal of Wound Ostomy and Continence Nurses 2014;41(5):424-429.
Pitti G, Clemente-Skurulsky C, Garner B, Gayden S. Collaborative approach to reduce respiratory medical device related pressure ulcers. Poster presentation at the Symposium on Advanced Wound Care (Fall), Las Vegas, Nevada, United States of America, 2013.
Rodzen LT, Stunkard J. Standardization and transparency drives down pressure injuries. Poster presentation at National Pressure Ulcer Advisory Panel Biennial Conference, New Orleans, Louisiana, United States of America, 2017.
Ruben B, Armstead S. Post operative tracheostomy protocol for obese and low Braden score patients in ICU setting. Poster presentation at the Joint Conference of the Wound Ostomy and Continence Nurses Society and the World Council of Enterostomal Therapists, Phoenix, Arizona, United States of America, 2010.
Santamaria N, Gerdtz M, Liu W, Rakis S, Sage S, Ng AW, Tudor H, McCann J, Vassiliou T, Morrow F, Smith K, Knott J, Liew D. Clinical effectiveness of a silicone foam dressing for the prevention of heel pressure ulcers in critically ill patients: Border II Trial. Journal of Wound Care 2015;24(8).
Sullivan S. A two-year retrospective review of suspected deep tissue injury evolution in adult acute care patients. Ostomy Wound Management 2013;59(9):30-39.
Tamburino J, McGrath M, Cooper M, McLeod B, Binns, M. A quality improvement initiative focusing on high risk left ventricular device patients; a combination of people, process, and technology. Poster presentation at the 46th Annual Conference of the Wound Ostomy and Continence Nurses' Society, Nashville, Tennessee, United States of America, 2014.
Tariq G. Pressure ulcer prevalence and prevention in Sheikh Khalifa Medical City, Abu Dhabi. Wounds Middle East 2014;1(2):8-14.
Thorpe E. Prophylactic use of dressings for pressure ulcer prevention. British Journal of Nursing 2016;25(12):S6-S12.
Thul J, Valero, E. Sacral pressure ulcer prevention in trauma patients. Poster presentation at Wound Ostomy and Continence Nurses' Society conference, San Antonio, Texas, United States of America, 2015.
Walsh NS, Blanck AW, Smith L, Cross M, Andersson L, Polito C. Use of a sacral silicone border foam dressing as one component of a pressure ulcer prevention program in an intensive care unit setting. Journal of Wound Ostomy & Continence Nursing 2012;39(2):146-149.
Yoshimura M, Ohura N, Tanaka J, Ichimura S, Kasuya Y, Hotta O, Kagaya Y, Sekiyama T, Tannba M, Suzuki N. Soft silicone foam dressing is more effective than polyurethane film dressing for preventing intraoperatively acquired pressure ulcers in spinal surgery patients: the Border Operating room Spinal Surgery (BOSS) trial in Japan. International Wound Journal 2016; Dec 7. doi: 10.1111/iwj.12696.

At Mölnlycke, we are dedicated to helping you, help patients. Explore our range of innovative medical products and solutions.





