Double gloving for complete protection
In discussion with surgeons and other O.R. staff, such as surgical nurses, safety for their patients and for themselves is a key concern.

`I always double-glove, and have from the very beginning. It's never been a challenge to work this way.´
David Revez, Neurosurgeon
When asked about double gloving as a safety practice, no matter the type of surgery, there are mixed reactions. While all surgeons will exclaim, 'My hands are my everything!', 'My hands are an extension of all my years of training' or 'After my brain, my hands are the most important part of my body. Without my hands, I cannot do anything', the resistance to double gloving still exists among some surgeons, while others refuse to operate without using double gloves.
Any contact with blood introduces risk in the form of blood borne illnesses, such as hepatitis and HIV, which is why the use of surgical gloves was universally adopted in the first place. But knowing that glove punctures happen frequently (up to 45 percent in some types of surgery)
Protecting human investment
Why is this extra layer of safety important, and where does the resistance come from? Apart from the peace of mind and proven protection to staff and patient health that double gloving provides, double gloving is also a protective measure in other ways. For example, for a hospital, double-gloving practice and policy is a form of protecting its investment. How?
First and foremost, a surgeon's hands and training are his/her livelihood, and by extension, the "life blood" of the hospital. The training and work s/he has done at a hospital has a value. The same applies for the entire surgical staff. From a health economics perspective, double gloving protects hospital staff and the hospital by reducing risk.
Healthcare professionals who have sustained a sharps or needlestick injuries have explained the anxiety, sleeplessness and worry of waiting for days after exposure to blood to learn their status. They work with their hands and depend on having the most protection they can get. This kind of injury can lead to lost work time, potential emotional trauma for patient and staff and even legal action and financial consequences.
Post-exposure testing and preventive treatment can be expensive. According to four US healthcare facilities, the mean cost of managing an exposure to a patient with hepatitis C is USD 650, and exposure to an HIV-infected patient is 2,456
Another concern, of course, is the risk for and treatment of a surgical site infection, which can double the length of a patient’s hospital stay (average of 16.8 additional days) and require an extra week (7.4 days) of antibiotic therapy
Double gloving is a simple and effective way to reduce the cost of Occupational Exposure to percutaneous injuries.
Retrain the brain for protection: The last tactile mile
Quote by Julie Karlsson, Trauma Nurse: To clinicians who don´t double-glove, I say, 'Do it!'. It´s such a simple way to protect yourself and everyone else.The evidence shows the risks and costs, and the last piece of the puzzle is fighting against resistance to double gloving and providing more incentive to double glove. More surgeons and their staff need to protect themselves against the dangers and risks, starting with rethinking and retraining with an even more vigilant, evidence-based, safety-first approach.
Healthcare professionals indicate a need and want for extra protection, and this demand appears as a priority in legislation and recommendations. The Sharps Agenda in the US and the EU Sharps Directive (external link, opens in a new window) in Europe, for example, both recommend double gloving as a protective measure against sharps injuries and their real consequences. In conjunction, authorities such as the Centers for Disease Control and Prevention (CDC)
The last argument against – and often the last mile to go – in adopting double gloving is usually tactile sensitivity. Compared against the gains in safety, the loss of tactile sensitivity resulting from double gloving is insignificant. Performance is not compromised with double gloving; studies have shown that after an initial period of getting used to double gloving (most surgeons adapt fully within two days
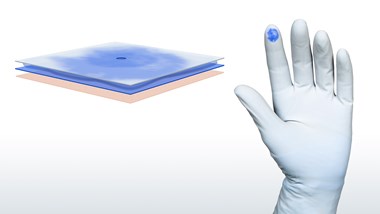
The next step in complete protection is adopting a double gloving puncture indication system. Double gloving with a coloured puncture indication system (with a clear, fast and large indicator for early detection and enabling quick action to reduce risk)
Related products
'References'